Massachusetts Alliance of Juvenile Court Clinics
(Line Item 5055-0000)
Every year, thousands of the Commonwealth’s most vulnerable, under-resourced children and families appear before the Massachusetts Juvenile Courts. Over 70% face a combination of mental health and behavioral problems, medical issues, substance use, histories of abuse and neglect, learning disabilities, and acculturation stressors. The Juvenile Court Clinics consult to the Court on the most complicated cases.
The Juvenile Court Clinics were established with the statewide Juvenile Court in 1993. The Juvenile Court continues to respond to changes brought about by the COVID-19 pandemic and Criminal Justice Reform Legislation passed in 2018 which changed the age of Juvenile Court jurisdiction on delinquency matters to age 12 to 18 (previously age 7 to 18) and expanded Diversion and Restorative Justice programs.
We want to thank the Legislature for appropriating an increase of $1.5 Million in FY25 to support the retention, recruitment and expansion of highly specialized clinical staff! This crucial funding will help alleviate the staffing crisis in the Juvenile Court Clinics as they serve the most vulnerable children and families in the Commonwealth, a population disproportionately represented in the Juvenile Court.
- Children suffering from trauma due to parental/caregiver neglect and abuse, violence in their schools, and/or are at-risk for sexual exploitation.
- Children exposed to cyberbullying, inappropriate content and exploitation through the Internet, resulting in mental health issues.
- Children with substance use problems requiring emergency out-of-home care through a court order or specialized help to access limited community-based outpatient services.
- Children with Autism Spectrum Disorder requiring specialized assessment to understand behaviors that could impact their involvement with the juvenile justice system.
- Children who are Dual-Status Youth, involvedin both the child welfare and the juvenile justice systems, and at-risk for further involvement with the juvenile justice system.
- Children with multiple, complex issues who fall between the cracks of state agencies such as DCF, DMH, DYS, DDS and DPH.
- Children with Child Requiring Assistance matters who have not improved despite intensive, comprehensive home-based services.
- Children who fail to meet criteria for Competence to Stand Trial and require repeat evaluations.
- Children boarding for days or weeks in hospital emergency rooms awaiting in-patient care.
- Parents before the Juvenile Court due to neglect and abuse of their children.
- Parents who require advocacy andguidanceto access services specific to their family’s unique needs.
The Role of the Juvenile Court Clinics
Psychologists, social workers, and other mental health professionals at the Juvenile Court Clinics provide court-ordered evaluations, interventions and referral services. All clinicians must be specially trained and credentialed by DMH. Since the pandemic, clinicians have been trained to provide all services via telehealth where appropriate. The Juvenile Court Clinics assist the Court in balancing the interests among child- or family-centered interventions, public safety, and protection of children from abuse and neglect, while providing the following:
- Emergency evaluations of youth in crisis—for example, an evaluation of a 15-year-old boy who threatened to kill himself while at Court, or a Section 35 evaluation of a 17-year-old girl brought in for an emergency substance use evaluation because of her opioid abuse while on the run.
- Comprehensive psychosocial evaluations—such as evaluating a 14-year-old boy with an extensive trauma history who injured another youth. During the evaluation, the clinician also works with the family, school and child-serving agencies in the community to seek appropriate treatment and service planning.
- Case management services—such as helping the Spanish-speaking family of a 13-year-old boy with chronic truancy navigate waitlists and other barriers to services such as language capacity, transportation and housing.
- Participation in diversionary, community-based initiatives—for example, in the Juvenile Detention Alternatives Initiative (JDAI), Dual-Status Youth (DSY) Programs, and System of Care (SOC) meetings.
- Evaluations to assess Competency to Stand Trial—for example, an evaluation of whether a 12-year-old boy, charged with assault and battery after he injured a classmate in a fight at school, could assist his lawyer in participating in his defense. The need for competency evaluations is rising as more youth come before the Juvenile Court with mental health issues, cognitive limitations and special needs as well as immaturity.
- Specialized risk assessments and evaluations of substance use, sexual offending, aggressive behavior and fire setting—behavior typically related to a range of complex underlying problems. All evaluations include recommendations for appropriate treatment.
- Specialized evaluations in Care and Protection cases. These include evaluations of parenting capacity, evaluations of mental health concerns, and competency of a parent to assist counsel in court proceedings.
- Consultation to the Court and the community—Consultation to families, schools, community providers, state agencies, and others regarding how the complex and rapidly changing service delivery systems may prevent a child’s further court involvement or the need for more intrusive and extensive interventions.
Cost Benefits of Juvenile Court Clinics
- Research indicates that saving one high-risk youth from heavy drug use, dropping out of school, and a life of crime saves society an average of $5 Million. Providing the Juvenile Court with recommendations for structured, community-based treatment and services that maintain public safety can prevent unnecessary detention, which has been estimated to cost the Commonwealth up to $193,278 annually per juvenile.
- Mental illnesses are serious medical illnesses that fall along a continuum of severity. Without treatment the consequences of mental illness for the individual and society are staggering—unnecessary disability, unemployment, substance use, homelessness, inappropriate incarceration, suicide, and wasted lives—costing the US economy $282 Billion annually in adverse economic outcomes, according to a 2024 Yale analysis of the economic toll of mental illness.
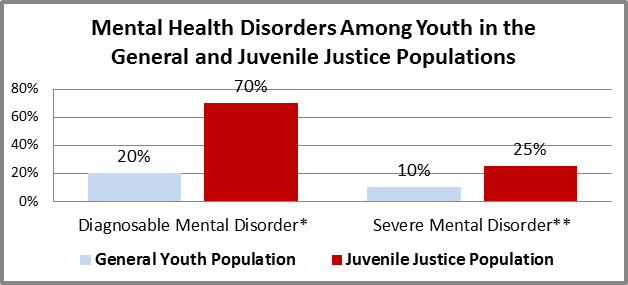
*An individual exhibiting behavioral or psychological symptoms that impact multiple life areas or create distress.
**A mental disorder so severe that an individual’s ability to perform routine daily tasks is significantly impaired.